The first transplant of human mini-kidneys into pigs opens a way to avoid wasting thousands of donated organs

Despite Spain being a world leader in organ transplants, thousands of people are left without the donated kidney they need each year. The same is true for other organs. Globally, the problem is far more serious, with millions affected and waiting lists that continue to grow due to the aging population. In the United States, seventeen people die every day waiting for a kidney transplant, and every nine minutes another patient is added to the waiting list. This situation threatens to overwhelm healthcare systems within a few years. Today, a biomedical breakthrough led by Spanish researchers opens a new avenue for alleviating transplant waiting lists using human mini-kidneys.
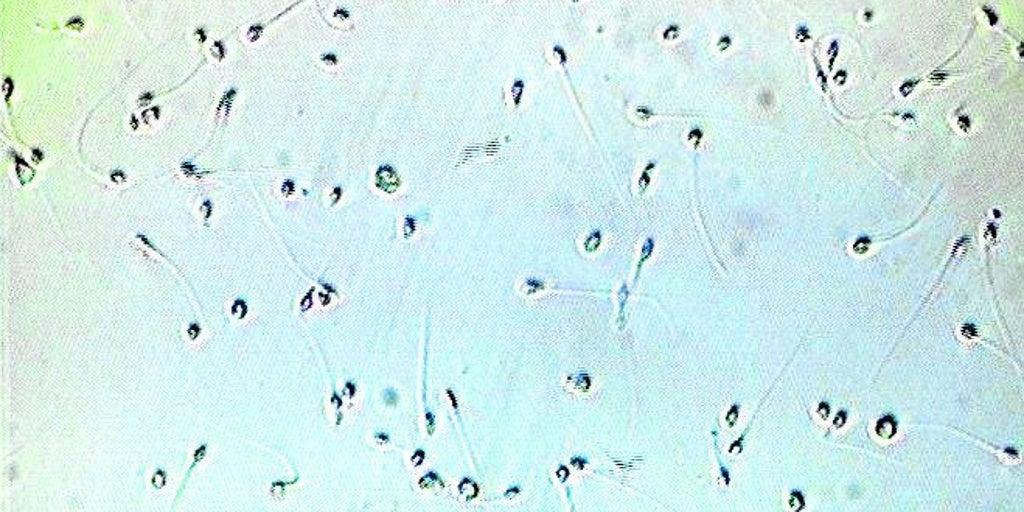
These organoids begin as a clump of a few stem cells, and then grow into tiny balls slightly smaller than the head of a pin. At that point, they already have a framework of specialized cells that resembles that of the different organs of the body, a characteristic that makes them ideal for studying diseases or conducting toxicology tests.
The new work takes a leap forward in exploring whether these structures can also be used for transplants in humans. The researchers have developed kidney organoids from human stem cells, cultured them, and, for the first time, demonstrated how to produce them in large quantities and cost-effectively, bringing their future application to patients closer.
The work has been directed by the 47-year-old Barcelona biologist Nuria Montserrat, ICREA research professor at the Institute for Bioengineering of Catalonia (IBEC) until just over a year ago, and current Minister of Research and Universities of the Government of Catalonia.
Before assuming her position in Salvador Illa's government, Montserrat had spent over a decade promoting the use of these cell cultures in regenerative medicine. Now, together with scientists from several Spanish institutions, including the National Transplant Organization, and researchers from the University of California, her team has successfully grafted human kidney organoids onto pig kidneys for the first time using normothermic perfusion machines, commonly used in the operating room to keep the organ alive and oxygenated outside the body before transplantation. This technique allows the integration of human cells into the animal's organ. For the first time, the researchers have re-transplanted these kidneys into the live animals from which they had been removed, demonstrating their functionality and the absence of rejection. The study was published this Friday in the specialized journal Nature Biomedical Engineering .
The next step, Montserrat explains to EL PAÍS, is to test the technique using organs from human cadavers. “Every year, more than 1,000 kidneys are discarded because they are unsuitable for transplantation. Now we have the opportunity to use them for research.” The ultimate goal is to reduce transplant waiting lists and increase the number of kidneys available for transplantation.
Manufacturing human organoids suitable for these uses is extremely complex. “Ten years ago,” Montserrat explains, “our idea was to create an entire human kidney from scratch, but that was very naive.” “The kidney is one of our most complex organs, with 23 different types of specialized cells,” she adds.

The new kidney organoids are barely visible when integrated into pig organs—they must measure about 200 microns to fit through the arteries without obstructing them—but they already contain 19 different types of specific cells. Thanks to collaboration with institutions across Spain, which form the backbone of a future network (development of mini-organs in Barcelona, experiments and transplants into pigs in A Coruña using perfusion machines manufactured in Zaragoza, and analysis of the immune response at the Carlos III Health Institute in Madrid), this technique has been demonstrated as a proof of concept.
The global organ shortage has driven the use of pig organs for human transplants. Until now, one of the most successful cases had been that of Tim Andrews, a 67-year-old American who received a pig kidney transplant that had been genetically modified to eliminate viruses and make it more compatible with his body. The operation was a success until just a few days ago, when doctors at Massachusetts General Hospital removed it because it was causing problems . Andrews lived 271 days with the implant, a world record. The first two patients to receive these transplants died shortly after the procedure, and the third was able to have it for 130 days before his body rejected it. Other living patients have also received experimental heart and liver transplants from these animals, although their effectiveness is still highly uncertain. For now, these types of procedures are seen as a bridge to buy time until the necessary human organ becomes available.
Human organoids are now emerging as a new avenue, according to Jordi Ochando , an immunologist at Carlos III University and Mount Sinai Hospital in New York, and co-author of the study. “Often, a patient receives not one, but several kidney transplants due to rejection. These techniques could help make grafts more compatible with the patient and prevent problems,” he explains. Furthermore, these analogs “can be used in human kidneys that are discarded for transplantation to increase the number of available organs, but they can also be used in transgenic pig kidneys to make them more compatible with the recipient,” he elaborates.
This is the first time that high-quality mini-kidneys have been produced in large quantities and with high reliability, highlights biochemist Elena Garreta , co-author of the study. “Until now, with conventional methods, you could create about 40 of these tissues. Now, thanks to our system, we can manufacture 30,000 in a single experiment, and we also verified that they are all of high quality,” she points out. There are still years of work ahead, but this advance opens many doors to therapeutic applications, she believes.
Nephrologist Beatriz Domínguez-Gil , director of the National Transplant Organization (ONT) and co-author of the study, paints the backdrop for this research. “On any given day, in Europe, there are more than 77,000 patients waiting for a kidney transplant, according to a recent study in 40 countries. These are people destined for long-term dialysis treatment, with the disruption this causes to their personal and professional lives. This is completely transformed by a kidney transplant , which improves life expectancy and is also less expensive than dialysis. This situation is complicated by the progressive aging of donors, who have greater comorbidity. This makes it essential to seek alternative solutions, and organoids are one of the possibilities for the future,” she explains. The director of the ONT explains that there is already an agreement with hospitals in Barcelona, Madrid, Galicia, and Cantabria to begin using discarded human organs in this research, presumably next year.
Although the application of these human tissues is still far off, Domínguez-Gil believes, the doctor predicts two uses for this technology: being able to remove the kidney of a person with kidney disease, treat it with a system similar to that used with pigs and reimplant it; and using this technique to regenerate donated organs that do not meet the requirements for transplantation.
Brazilian physician Leonardo Riella led the team that performed the pig kidney transplant on the American patient at Massachusetts General Hospital. The head of kidney transplantation and professor at Harvard University, who was not involved in this work, praises it as a great first step. “It is an elegant and innovative proof of concept demonstrating that human kidney organoids can survive and integrate within pig kidneys for a short period. It is an exciting step toward the convergence of regenerative medicine and xenotransplantation [from animal to human]. The main challenges going forward will be achieving long-term viability and demonstrating true kidney function from the transplanted organoids. If the latter is achieved, it could eventually lead to new treatments to restore kidney function in patients with chronic kidney disease,” he emphasizes.
Marcos López-Hoyos, head of immunology at the Marqués de Valdecilla University Hospital in Santander, cautions that these techniques are still in the animal research phase, but are nonetheless “very interesting.” “Kidneys are already being recovered using ex vivo perfusion methods like those used in this study. Organoids, while not a complete replica of a real kidney, are capable of regenerating it and offer enormous potential for treatment,” he emphasizes.
EL PAÍS